Abstract
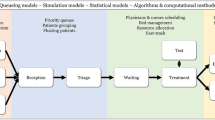
Inefficient management of emergent surgeries in hospitals can, in part, be attributed to a lack of rigorous analysis appropriate to capturing the underlying uncertainties inherent to this process and a pricing mechanism to ensure its financial viability. We develop a non-preemptive multi-priority queueing model that optimally manages emergent surgeries and supports the resource allocation decision-making process. Specifically, we utilize queueing and discrete event simulation to develop empirical models for determining the required number of emergent operating rooms for a hospital surgical department. We also present algorithms that estimate the appropriate pricing for patient surgeries differentiated by priority level given the patient demand and the resources reserved to meet this demand.





Similar content being viewed by others
Notes
The findings might not hold if the surgery distribution did not fit a γ-type distribution (of which the Erlang is a special case), in which the distribution averages are additive.
References
Albright SC, Winston WL and Zappe CJ (2009). Data Analysis and Decision Making, 4/e. South-Western Cengage Learning: Mason, OH.
Blake JT, Dexter F and Donald J (2002). Operating rooms managers’ use of integer programming for assigning block time to surgical groups: A case study. Anesthesia & Analgesia 94 (1): 143–148.
Cardoen B, Demeulemeester E and Beliën J (2010). Operating room planning and scheduling: A literature review. European Journal of Operational Research 201 (3): 921–932.
Cohen J (1988). Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum Associates: Hillsdale, NJ.
Denton B, Rahman AS, Nelson H and Bailey AC (2006). Simulation of a multiple operating room surgical suite. In: Perrone LF, Wieland FP, Liu J, Lawson BG, Nicol DM and Fujimoto RM (eds). Proceedings of the 2006 Winter Simulation Conference, Monterey, pp 414–424.
Denton B, Viapiano J and Vogl A (2007). Optimization of surgery sequencing and scheduling decisions under uncertainty. Health Care Management Science 10 (1): 13–24.
Gerchak Y, Gupta D and Henig M (1996). Reservation planning for elective surgery under uncertain demand for emergency surgery. Management Science 42 (3): 321–334.
Goldman J and Knappenberger H (1968). How to determine the optimum number of operating rooms. Modern Hospital 111 (3): 114–116.
Guerriero F and Guido R (2011). Operational research in the management of the operating theatre: A survey. Health Care Management Science 14 (1): 89–114.
HFMA (2003). Achieving operating room efficiency through process integration. Health Care Financial Management 57 (3): S1–S7.
HFMA (2004). Strategic price setting: ensuring your financial viability through price modeling. Health Care Financial Management 58 (7): 1–7.
Jebali A, Hadj Alouane AB and Ladet P (2006). Operating rooms scheduling. International Journal of Production Economics 99 (1–2): 52–62.
Lamiri ML, Xie D and Zhang S (2008). Column generation approach to operating theater planning with elective and emergency patients. IIE Transactions 40 (9): 838–852.
Levtzion-Korach O, Murphy KG, Madden S and Dempsey C (2010). For urgent and emergent cases, which one goes to the OR first? OR Manager 26 (7): 1,11–13.
Litvak E and Long MC (2000). Cost and quality under managed care: Irreconcilable differences? American Journal of Managed Care 6 (3): 305–312.
Litvak E, Long MC, Cooper AB and McManus ML (2001). Emergency department diversion: causes and solutions. Academic Emergency Medicine 8 (11): 1108–1110.
Ozkarahan I (2000). Allocation of surgeries to operating rooms by goal programming. Journal of Medical Systems 24 (6): 339–378.
Pai J-Y, Petry F and Fos P (1997). Employing simulation to optimize the number of operating rooms in hospitals. Technical Report. In: Proceedings of the Medical Sciences Simulation Conference. The Society for Computer Simulation International (SCS): Phoenix, pp 36–42.
Persson MJ and Persson JA (2010). Analysing management policies for operating room planning using simulation. Health Care Management Science 13 (2): 182–191.
ProModel (2010). Software website, http://www.promodel.com, accessed May 2010.
Sier D, Tobin P and McGurk C (1997). Scheduling surgical procedures. Journal of the Operational Research Society 48 (9): 884–891.
Stanciu A, Vargas L and May J (2010). A revenue management approach for managing operating room capacity. In: Johansson B, Jain S, Montoya-Torres J, Hugan J, and Yücesan E (eds). Proceedings of the 2010 Winter Simulation Conference. Baltimore, pp 2444–2454.
Ross SM (2003). Introduction to Probability Models, 8/e. Academic Press: San Diego, CA.
Tucker JB, Barone JE, Cecere J, Blabey RG and Rha CK (1999). Using queueing theory to determine operating room staffing needs. Journal of Trauma 46 (1): 71–79.
van Oostrum JM, et al (2008). A simulation model for determining the optimal size of emergency teams on call in the operating room at night. Anesthesia & Analgesia 107 (5): 1655–1662.
Wullink G, Houdenhoven MV, Hans EW, Oostrum JM, van der Lans M and Kazemier G (2007). Closing emergency operating rooms improves efficiency. Journal of Medical Systems 31 (6): 543–546.
Zhang B, Murali P, Dessouky MM and Belson D (2009). A mixed integer programming approach for allocating operating room capacity. Journal of the Operational Research Society 60 (5): 663–673.
Zonderland ME, Boucherie RJ, Litvak N and Vleggeert-Lankamp C (2010). Planning and scheduling of semi-urgent surgeries. Health Care Management Science 13 (3): 256–267.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix A
Effect of priority transition
For highest priority customers, the expected wait time without transitions is given as:

that is, the number of Priority 1 patients in the queue and the residual time for patients in service. With transition, Priority 1 would also have to wait for all the lower priority classes that have already waited longer than the difference in survivability time between the priorities, given as  , where Pm, n=P(wait time priority>ω
m
ω
n
), that is, the probability that priority ‘m’ has waited longer than the difference in wait time of priority ‘n’, where m>n which is strictly positive, thus the expected wait time for Priority 1 will be higher.
, where Pm, n=P(wait time priority>ω
m
ω
n
), that is, the probability that priority ‘m’ has waited longer than the difference in wait time of priority ‘n’, where m>n which is strictly positive, thus the expected wait time for Priority 1 will be higher.
For priorities >1 without transition, we can decompose the expected wait time into two components: the amount of residual service time of a patient currently in service as well as all patients with the same or higher priority in the queue upon arrival. The second is all the higher priority patients arriving during the patients waiting time:

Two additional terms account for the possibility of transition of priority resulting from excessive wait time. The first concerns the presence of lower priority patients that have waited longer than the difference between the survivability times. The second addresses the fact that arriving higher priority patients will only take priority for those priority ‘i’ patients that have not waited longer than the difference in survivability times. Adding these to the above equation results in

The second term increases the expected wait time, while the addition of (1−Pi, j) to the last term decreases the expected wait time, with the net effect dependent upon system dynamics. The only exception is for the lowest priority, as the second term is zero given that there are no lower priority patients. Thus, the lowest priority will always see a decrease in their expected wait time.
Appendix B
Rights and permissions
About this article
Cite this article
Paul, J., MacDonald, L. Determination of number of dedicated OR's and supporting pricing mechanisms for emergent surgeries. J Oper Res Soc 64, 912–924 (2013). https://doi.org/10.1057/jors.2012.92
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1057/jors.2012.92