Abstract
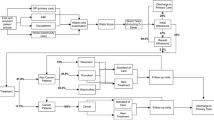
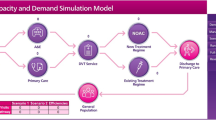
We provide a framework for simulating the entire patient journey across different phases (such as diagnosis, treatment, rehabilitation and long-term care) and different sectors (such as GP, hospital, social and community services), with the aim of providing better understanding of such processes and facilitating evaluation of alternative clinical and care strategies. A phase-type modelling approach is used to promote better modelling and management of the specific elements of a patient pathway, using performance measures such as clinical outcomes, patient quality of life, and cost. The approach is illustrated using stroke disease. Approximately 5% of the United Kingdom National Health Service budget is spent treating stroke disease each year. There is an urgent need to assess whether existing services are cost-effective or new interventions could increase efficiency. This assessment can be made using models across primary and secondary care; in particular we evaluate the cost-effectiveness of thrombolysis (clot busting therapy), using discrete event simulation. Using our model, patient quality of life and the costs of thrombolysis are compared under different regimes. In addition, our simulation framework is used to illustrate the impact of internal discharge queues, which can develop while patients are awaiting placement. Probabilistic Sensitivity Analysis of the value parameters is also carried out.







Similar content being viewed by others
References
Barton M, McClean S, Gillespie J, Garg L, Wilson D and Fullerton K (2012). Is it beneficial to increase the provision of thrombolysis— A discrete event simulation model. QJM: An International Journal of Medicine 105(7): 665–673.
Briggs AH, Weinstein MC, Fenwick E, Karnon J, Sculpher MJ and Paltiel AD (2012). Model parameter estimation and uncertainty: A report of the ISPOR-SMDM modeling good research practices task force-6. Value Health 15(6): 835–842.
Caro J (2005). Pharmacoeconomic analyses using discrete event simulation. Pharmoeconomics 23(4): 323–332.
Caro J, Moller J and Getsios D (2010). Discrete event simulation: The preferred technique for health economic evaluations? Value in Health 13(8): 1056–1060.
Caro JJ, Briggs AH, Siebert U and Kuntz KM (2012). Modeling good research practices-overview: A report of the ISPOR-SMDM modeling good research practices task force-1. Value Health 15(4): 796–803.
Cerner (2010). Patient administration systems, Cerner, London, http://www.cerner.com/solutions/Hospitals_and_Health_Systems/Patient_Administration_Systems/?LangType=2057, accessed 17 February 2015.
Crane GJ, Kymes SM, Hiller JE, Casson R, Martin A and Karnon JD (2013). Accounting for costs, QALYs and capacity constraints: Using discrete event simulation to evaluate alternative service delivery and organisational scenarios for hospital based Glaucoma services. Medical Decision Making 33(8): 986–997.
De Bruin AM, Van Rossum AC, Visser MC and Koole G (2007). Modeling the emergency cardiac in-patient flow: An application of queuing theory. Health Care Management Science 10(2): 125–137.
Dorman P, Dennis M and Sandercock P (2000). Are the modified ‘simple questions’ a valid and reliable measure of health related quality of life after stroke? J Neurol Neurosurg Ps 69(4): 487–493.
Dronne M et al (2004). Mathematical modelling of an ischemic stroke: An integrative approach. Acta Biotheoretica 52(4): 255–272.
Eddy DM, Hollingworth W, Caro JJ, Tsevat J, McDonald KM and Wong JB (2012). Model transparency and validation: A report of the ISPOR-SMDM modeling good research practices task force-7. Value Health 15(6): 843–850.
Fackrell M (2009). Modelling healthcare systems with phase-type distributions. Health Care Management Science 12(1): 11–26.
Fine S, Singer Y and Tishby N (1998). The hierarchical hidden Markov model: Analysis and applications. Machine Learning 32(1): 41–62.
Garg L, McClean S, Barton M, Meenan BJ and Fullerton K (2012). Intelligent patient management and resource planning for complex, heterogeneous, and stochastic healthcare systems. IEEE Transactions on Systems, Man and Cybernetics— Part A Systems and Humans 42(6): 1332–1345.
Garg L, Mulvaney A, Gupta V and Calleja N (2015). Phase-type survival trees for hospital bed occupancy and requirements forecasting. The 22nd EurOMA International Annual Conference (EurOMA 2015), 26 June–1 July. Neuchâtel, Switzerland, HOM-16.
Gillespie J, McClean S, Scotney B, Garg L, Barton M and Fullerton K (2011). Costing hospital resources for stroke patients using phase-type models. Health Care Management Science 14(3): 279–291.
Griffiths JD, Williams JE and Wood RM (2013). Modelling activities at a neurological rehabilitation unit. European Journal of Operational Research 226(2): 301–312.
Karnon J, Stahl J, Brennan A, Caro JJ, Mar J and Möller J (2012). Modeling using discrete event simulation: A report of the ISPOR-SMDM modeling good research practices task force-4. Value Health 15(6): 821–827.
Kent D, Selker H, Ruthazer R, Bluhmki E and Hacke W (2006). The stroke-thrombolytic predictive instrument: A predictive instument for intraveneous thrombolysis in acute ischemic stroke. Stroke 37(12): 2957–2962.
Knight VA and Harper PR (2012). Modelling emergency medical services with phase-type distributions. Health Systems 1(1): 58–68.
Langhorne P (2007). Organised inpatient (stroke unit) care for stroke. Cochrane Database of Systematic Reviews 4(1): 1–43.
Marshall AH and Zenga M (2012). Experimenting with the Coxian phase-type distribution to uncover suitable fits. Methodol Comput Appl Probab 14(1): 71–86.
McClean SI, Barton M, Garg L and Fullerton K (2011). A modeling framework that combines markov models and discrete-event simulation for stroke patient care. ACM Transactions on Modeling and Computer Simulation (TOMACS) 21(4): 1–26.
McClean S, Garg L and Fullerton K (2014b). Costing mixed Coxian phase-type systems with poisson arrivals. Communications in Statistics—Theory and Methods 43(7): 1437–1452.
McClean S, Gillespie J, Garg L, Barton M, Scotney B and Fullerton K (2014a). Using phase-type models to cost stroke patient care across health, social and community services. European Journal of Operational Research 236(1): 190–199.
McClean S, Gillespie J, Scotney B and Fullerton K (2012). Using phase-type models to cost a cohort of stroke patients. IEEE International Conference on Computer Based Medical Systems, Rome, Italy.
National Institute for Health and Care Excellence (NICE) (2013). ‘Guide to the methods of technology appraisal’, http://www.nice.org.uk/article/pmg9/resources/non-guidance-guide-to-the-methods-of-technology-appraisal-2013-pdf, accessed 2 April 2016.
National Institute for Health Excellence and Clinical Excellence (NICE) (2015). ‘The NICE Glossary’, http://www.nice.org.uk/glossary, accessed 17 February 2015.
Neil N (2012). Transparently, with validation. Med Decis Making 32(5): 660–662.
Nguyen NT, Phung DQ, Venkatesh S and Bui HH (2005). Learning and detecting activities from movement trajectories using the hierarchical hidden Markov models. In Proceedings of the 2005 IEEE Computer Society Conference on Computer Vision and Pattern Recognition (CVPR'05). Volume. 2, IEEE Computer Society: Washington, DC, USA, pp 955–960.
Pari AA, Simon J, Wolstenholme J, Geddes JR and Goodwin GM (2014). Economic evaluations in bipolar disorder: A systematic review and critical appraisal. Bipolar Disorders 16(6): 557–582.
Penaloza-Ramos MC et al (2014). Cost-effectiveness of optimizing acute stroke care services for thrombolysis. Stroke 45(2): 553–562.
Personal Social Services Research Unit (PSSRU) (2006). Unit costs of health and social care, pp 1–230. London, http://www.pssru.ac.uk/pdf/uc/uc2006/uc2006.pdf, accessed 17 February 2015.
Pilgrim H et al (2009). The costs and benefits of bowel cancer service developments using discrete event simulation. Journal of the Operational Research Society 60(10): 1305–1314.
Rabiner LR (1989). A tutorial on hidden Markov models and selected applications in speech recognition. Proceedings of the IEEE 77(2): 257–286.
Roberts M, Russel L, Paltiel AD, Chambers M, McEwan P and Krahn M (2012). Conceptualizing a model: A report of the ISPOR-SMDM modeling good research practices task force-2. Value Health 15(6): 804–811.
Royal College of Physicians National Sentinel Stroke Audit Report (RCP) (2011). Audit of stroke, pp 1–69. London, https://www.rcplondon.ac.uk/sites/default/files/national-sentinel-stroke-audit-2010-public-report-and-appendices_0.pdf, accessed 17 February 2015.
Sackley C and Pound K (2002). Setting priorities for a discharge plan for stroke patients entering nursing home care. Clinical Rehabilitation 16(8): 859–866.
Saka O, McGuire A and Wolfe C (2009). Cost of stroke in the United Kingdom. Age and Ageing 38(1): 27–32.
Sandercock P et al (2002). A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischemic stroke in the NHS. Health Technology Assessment 26(6): 1–112.
Siebert U et al (2012). State-transition modeling: A report of the ISPOR-SMDM modeling good research practices task force-3. Value Health 15(6): 812–820.
Stevenson MD, Brazier JE, Calvert NW, Lloyd-Jones M, Oakley JE and Kanis JE (2005). Description of an individual patient methodology for calculating the cost-effectiveness of treatments for osteoporosis in woman. Journal of the Operational Research Society 56(2): 214–221.
Sudlow C and Wardlow C (2009). Getting the priorities right for stroke care. BMJ 338(7708): 1419–1422.
Sundberg G, Bagust A and Terent A (2003). A model for costs of stroke services. Health Policy 63(1): 81–94.
Tang X, Luo Z and Gardiner JC (2012). Modeling hospital length of stay by Coxian phase-type regression with heterogeneity. Statistics in Medicine 31(14): 1502–1516.
Taylor GJ, McClean SI and Millard PH (1998). Using a continuous-time Markov model with poisson arrivals to describe the movement of geriatric patients. Applied Stochastic Models in Business and Industry 14(2): 165–174.
The National Institute of Neurological Disorders and stroke rt-PA Stroke Study Group (NINDS) (1995). Tissue plasminogen activator for acute ischemic stroke. New England Journal of Medicine 333(24): 1581–1588.
Thi V, Duong DQ, Phung H, Hai B and Svetha V (2009). Efficient duration and hierarchical modeling for human activity recognition. Artif. Intell 173(7–8): 830–856.
Tsoi AC, Zhang S and Hagenbuchner M (2005). Pattern discovery on Australian medical claims data-A systematic approach. IEEE Trans. Knowl. Data Eng 17(10): 1420–1435.
Tsoi AC, Zhang S and Hagenbuchner M (2006). Hierarchical hidden Markov models: An application to health insurance data. In. Data Mining: Theory, Methodology, Techniques, and Applications, Volume 3755 of the series Lecture Notes in Computer Science. Springer: Berlin, Heidelberg, pp 244–259.
van Karnebeek CDM et al (2015). Health economic evaluation of plasma oxysterol screening in the diagnosis of Niemann—Pick type C disease among intellectually disabled using discrete event simulation. Molecular Genetics and Metabolism 114(2): 226–232.
Wahlgren N et al (2008). Multivariable analysis of outcome predictors and adjustment of main outcome results to baseline data profile in randomized controlled trials: Safe implementation of thrombolysis in stroke-monitoring study. Stroke 39(12): 3316–3322.
Xie H, Chaussalet TJ and Millard PH (2006). A model-based approach to the analysis of patterns of length of stay in institutional long-term care. IEEE Transactions on Information Technology in Biomedicine 10(3): 512–518.
Youngblood MG and Cook DJ (2007). Data mining for hierarchical model creation. IEEE Transactions on Systems, Man, and Cybernetics, Part C 37(4): 561–572.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gillespie, J., McClean, S., Garg, L. et al. A multi-phase DES modelling framework for patient-centred care. J Oper Res Soc 67, 1239–1249 (2016). https://doi.org/10.1057/jors.2015.114
Published:
Issue Date:
DOI: https://doi.org/10.1057/jors.2015.114