Abstract
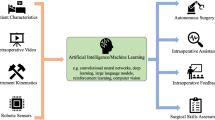
Virtual reality (VR) medical simulations deliver a tailored learning experience that can be standardized, and can cater to different learning styles in ways that cannot be matched by traditional teaching. These simulations also facilitate self-directed learning, allow trainees to develop skills at their own pace and allow unlimited repetition of specific scenarios that enable them to remedy skills deficiencies in a safe environment. A number of simulators have been validated and have shown clear benefits to medical training. However, while graphical realism is high, realistic haptic feedback and interactive tissues are limited for many simulators. This paper reviews the current status and benefits of haptic VR simulation-based medical training for bone and dental surgery, intubation procedures, eye surgery, and minimally invasive and endoscopic surgery.


Similar content being viewed by others
References
Abrahamson S, Denson J and Wolf R (2004). Effectiveness of a simulator in training anesthesiology residents. Quality and Safety in Health Care 13 (5): 395–397.
Allard J et al (2007). SOFA—An Open Source Framework for Medical Simulation. Medicine Meets Virtual Reality 15. IOS Press: Long Beach, CA, pp 13–18.
Barach P and Johnson JK (2009). Reducing variation in adverse events during the academic year. British Medical Journal 339 (1): 3949.
Barry-Issenberg S, McGaghie W, Petrusa E, Lee Gordon D and Scalese R (2005). Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Medical Teacher 27 (1): 10–28.
Basdogan C, Ho CH and Srinivasan MA (1999). Simulation of tissue cutting and bleeding for laparoscopic surgery using auxiliary surfaces. Studies in Health Technology and Informatics 62: 38–44.
Bashankaev B, Baido S and Wexner S (2011). Review of available methods of simulation training to facilitate surgical education. Surgical Endoscopy 25 (1): 28–35.
Berkley J, Turkiyyah G, Berg D, Ganter M and Weghorst S (2004). Real-time finite element modeling for surgery simulation: An application to virtual suturing. IEEE Trans Vis Comput Graph 10 (3): 314–325.
Buchanan JA (2004). Experience with virtual reality-based technology in teaching restorative dental procedures. Journal of Dental Education 68 (12): 1258–1265.
Chalasani V, Cool DW, Sherebrin S, Fenster A, Chin J and Izawa JI (2011). Development and validation of a virtual reality transrectal ultrasound guided prostatic biopsy simulator. Can Urol Assoc J 5 (1): 19–26.
Choi C, Han H, An B and Kim J (2006). Development of a surgical simulator for laparoscopic esophageal procedures. Conference Proceedings of the Engineering in Medicine and Biology Society 1 (1): 819–822.
Coles T, Meglan D and John N (2011). The role of haptics in medical training simulators: A survey of the state of the art. IEEE Transactions on Haptics 4 (1): 51–66.
Cooke M, Irby D, Sullivan W and Ludmerer K (2006). American medical education 100 years after the flexner report. New England Journal of Medicine 355 (13): 1339–1344.
Cotin S et al (2005). Collaborative development of an open framework for medical simulation. MICCAI Open-Source Workshop. Vol. 34. Copenhagen.
Crassin C, Neyret F, Lefebvre S and Eisemann E (2009). GigaVoxels: Ray-guided streaming for efficient and detailed voxel rendering. Proceedings of the 2009 Symposium on Interactive 3D Graphics and Games. ACM: Boston, MA, pp. 15–22.
De Visser H et al (2010). Developing a next generation colonoscopy simulator. International Journal of Image and Graphics 10 (2): 203–217.
Ericsson K (2004). Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Academic Medicine 79 (10): 70.
Feudner EM, Engel C, Neuhann IM, Petermeier K, Bartz-Schmidt KU and Szurman P (2009). Virtual reality training improves wet-lab performance of capsulorhexis: Results of a randomized, controlled study. Graefes Archive for Clinical and Experimental Ophthalmology 247 (7): 955–963.
Gallagher A and Cates C (2004). Virtual reality training for the operating room and cardiac catheterisation laboratory. The Lancet 364 (9444): 1538–1540.
Goswami P, Schlegel P, Solenthaler B and Pajarola R (2010). Interactive SPH simulation and rendering on the GPU. Proceedings of the 2010 ACM SIGGRAPH/Eurographics Symposium on Computer Animation. Eurographics Association: Madrid, Spain, pp. 55–64.
Grantcharov T, Kristiansen V, Bendix J, Bardram L, Rosenberg J and Funch-Jensen P (2004). Randomized clinical trial of virtual reality simulation for laparoscopic skills training. British Journal of Surgery 91 (2): 146–150.
Haller G, Myles PS, Taffe P, Perneger TV and Wu CL (2009). Rate of undesirable events at beginning of academic year: Retrospective cohort study. British Medical Journal 339 (1): 3974.
Haluck R and Krummel T (2000). Computers and virtual reality for surgical education in the 21st century. Archives of Surgery 135 (7): 786.
Harders M, Bajka M, Spaelter U, Tuchschmid S, Bleuler H and Székely G (2005a). Highly-realistic, immersive training environment for hysteroscopy. Studies in Health Technology and Informatics 119: 176.
Harders M, Steinemann D, Gross M and Szekely G (2005b). A hybrid cutting approach for hysteroscopy simulation. Lecture Notes in Computer Science 3750 (2): 567.
Heinrichs WL, Srivastava S, Dev P and Chase RA (2004). LUCY: A 3-D pelvic model for surgical simulation. Journal of the American Association of Gynecologic Laparoscopists 11 (3): 326–331.
Heng PA et al (2004). A virtual-reality training system for knee arthroscopic surgery. IEEE Transactions on Information Technology in Biomedicine 8 (2): 217–227.
Hikichi T et al (2000). Vitreous surgery simulator. Archives of Ophthalmology 118 (12): 1679.
Ikonen T, Antikainen T, Silvennoinen M, Isojärvi J, Mäkinen E and Scheinin T (2012). Virtual reality simulator training of laparoscopic cholecystectomies—A systematic review. Scandinavian Journal of Surgery 101 (1): 5–12.
Jackson A et al (2002). Developing a virtual reality environment in petrous bone surgery: A state-of-the-art review. Ontology & Neurotology 23 (2): 111–121.
Kallstrom R, Hjertberg H, Kjolhede H and Svanvik J (2005). Use of a virtual reality, real-time, simulation model for the training of urologists in transurethral resection of the prostate. Scandinavian Journal of Urology and Nephrology 39 (4): 313–320.
Khalifa Y, Bogorad D, Gibson V, Peifer J and Nussbaum J (2006). Virtual reality in ophthalmology training. Survey of Ophthalmology 51 (3): 259–273.
Kurenov SN, Punak S, Kim M, Peters J and Cendan JC (2006). Simulation for training with the Autosuture Endo Stitch device. Surgical Innovation 13 (4): 283–287.
Laurell C, Söderberg P, Nordh L, Skarman E and Nordqvist P (2004). Computer-simulated phacoemulsification. Ophthalmology 111 (4): 693–698.
LeBlanc VR, Urbankova A, Hadavi F and Lichtenthal RM (2004). A preliminary study in using virtual reality to train dental students. Journal of dental education 68 (3): 378–383.
Lee W (1980). The acquisition of clinical ward skills during undergraduate medical training. Journal of Medical Education 55 (12): 1029–1031.
Lim F, Brown I, McColl R, Seligman C and Alsaraira A (2006). A visual graphic/haptic rendering model for hysteroscopic procedures. Journal of the Australasian College of Physical Scientists and Engineers in Medicine 29 (1): 57–61.
Luengo V, Larcher A and Tonetti J (2011). Design and implementation of a visual and haptic simulator in a platform for a TEL system in percutaneuos orthopedic surgery. Studies in health technology and informatics 163: 324–328.
Maciel A, Halic T, Lu Z, Nedel LP and De S (2009). Using the PhysX engine for physics-based virtual surgery with force feedback. International Journal of Medical Robotics 5 (3): 341–353.
Maciel A, Liu Y, Ahn W, Singh TP, Dunnican W and De S (2008). Development of the VBLaST: A virtual basic laparoscopic skill trainer. International Journal of Medical Robotics 4 (2): 131–138.
Mahr MA and Hodge DO (2008). Construct validity of anterior segment anti-tremor and forceps surgical simulator training modules: Attending versus resident surgeon performance. Journal of Cataract & Refractive Surgery 34 (6): 980–985.
Mayrose J, Kesavadas T, Chugh K, Joshi D and Ellis D (2003). Utilization of virtual reality for endotracheal intubation training. Resuscitation 59 (1): 133–138.
Moody L, Arthur J, Zivanovic A and Waterworth A (2003). A part-task approach to haptic knee arthroscopy training. Studies In Health Technology and Informatics 94: 216–218.
Morris D, Girod S, Barbagli F and Salisbury K (2005). An interactive simulation environment for craniofacial surgical procedures. Studies in Health Technology and Informatics 111: 334–341.
Morris D, Sewell C, Blevins N, Barbagli F and Salisbury K (2004). A collaborative virtual environment for the simulation of temporal bone surgery. In: Westwood JD et al (eds.). Medical Image Computing and Computer-Assisted Intervention (MICCAI). Springer: Rennes, France: 3 319–327.
Niederer P, Weiss S, Caduff R, Bajka M, Szekely G and Harders M (2009). Uterus models for use in virtual reality hysteroscopy simulators. European Journal of Obstetrics & Gynecology and Reproductive Biology 144 (Suppl 1): S90–S95.
Okrainec A et al (2009). Development of a virtual reality haptic Veress needle insertion simulator for surgical skills training. Studies In Health Technology and Informatics 142: 233–238.
Owens JD, Houston M, Luebke D, Green S, Stone JE and Phillips JC (2008). GPU Computing. Proceedings of the IEEE. IEEE: USA, 96(5): 879–899.
Padilla MA, Altamirano F, Arambula F and Marquez J (2007). Mechatronic resectoscope emulator for a surgery simulation training system of the prostate. Conference Proceedings of the IEEE Engineering in Medicineand Biology Society 2007 1750–1753.
Pedowitz RA, Esch J and Snyder S (2002). Evaluation of a virtual reality simulator for arthroscopy skills development. Arthroscopy 18 (6): E29.
Pohlenz P et al (2010). Virtual dental surgery as a new educational tool in dental school. Journal of Cranio-Maxillofacial Surgery 38 (8): 560–564.
Pories WJ, Smout JC, Morris A and Lewkow VE (1994). U.S. health care reform: Will it change postgraduate surgical education? World Journal of Surgery 18 (5): 745–752.
Privett B, Greenlee E, Rogers G and Oetting TA (2010). Construct validity of a surgical simulator as a valid model for capsulorhexis training. Journal of Cataract & Refractive Surgery 36 (11): 1835–1838.
Rhienmora P (2010). Haptic augmented reality dental trainer with automatic performance assessment, http://dl.acm.org/citation.cfm?id=1720054, accessed 20 July 2011.
Roberts K, Bell R and Duffy A (2006). Evolution of surgical skills training. World Journal of Gastroenterology 12 (20): 3219.
Rodrigues M, Gillies D and Charters P (1998). Modelling and simulation of the tongue during laryngoscopy. Computer Networks and ISDN Systems 30 (20–21): 2037–2045.
Rodrigues M, Gillies D and Charters P (2000). A biomechanical model of the upper airways for simulating laryngoscopy. Computer Methods in Biomechanics and Biomedical Engineering 4 (2): 127–148.
Rodrigues M, Gillies D and Charters P (2001). Realistic Deformable Models for Simulating the Tongue during Laryngoscopy. International Workshop on Medical Imaging and Augmented Reality. IEEE: USA.
Ruthenbeck GS, Hobson J, Carney AS, Sacks R and Reynolds KJ (2013). Towards photorealism in endoscopic sinus surgery simulation. American Journal of Rhinology and Allergy 27 (1): 6–12.
Ruthenbeck GS, Tan SB, Carney AS, Hobson JC and Reynolds KJ (2012). A virtual-reality subtotal tonsillectomy simulator. Journal of Laryngology & Otology 126 (Suppl 2): S8–S13.
Samosky J et al (2011). Toward a comprehensive hybrid physical-virtual reality simulator of peripheral anesthesia with ultrasound and neurostimulator guidance. Studies in Health Technology and Informatics 163: 552.
Samur E, Flaction L, Spaelter U, Bleuler H, Hellier D and Ourselin S (2008). A haptic interface with motor/brake system for colonoscopy simulation. The 2008 Symposium on Haptic Interfaces for Virtual Environment and Teleoperator Systems, IEEE Computer Society: USA.
Schijven M and Jakimowicz J (2003). Virtual reality surgical laparoscopic simulators. Surgical Endoscopy 17 (12): 1943–1950.
Schuppe O, Wagner C, Koch F and Manner R (2009). EYESi ophthalmoscope—A simulator for indirect ophthalmoscopic examinations. Studies in Health Technology and Informatics 142: 295–300.
Seevinck J et al (2006). A simulation-based training system for surgical wound debridement. Studies in Health Technology and Informatics 119: 491–496.
Selvander M and Asman P (2012). Virtual reality cataract surgery training: Learning curves and concurrent validity. Acta Ophthalmologica 90 (5): 412–417.
Serra L et al (1998). Multimodal volume-based tumor neurosurgery planning in the virtual workbench. Medical Image Computing and Computer-Assisted Intervention. Lecture Notes in Computer Science: Springer, Vol. 1496, pp 1007–1015.
Seymour N (2008). VR to OR: A review of the evidence that virtual reality simulation improves operating room performance. World Journal of Surgery 32 (2): 182–188.
Seymour N et al (2002). Virtual reality training improves operating room performance: Results of a randomized, double-blinded study. Annals of Surgery 236 (4): 458–464.
Sinclair MJ, Peifer JW, Haleblian R, Luxenberg MN, Green K and Hull DS (1995). Computer-simulated eye surgery. A novel teaching method for residents and practitioners. Ophthalmology 102 (3): 517–521.
Solomon B et al (2011). Simulating video-assisted thoracoscopic lobectomy: A virtual reality cognitive task simulation. Journal of Thoracic and Cardiovascular Surgery 141 (1): 249–255.
Sowerby LJ, Rehal G, Husein M, Doyle PC, Agrawal S and Ladak HM (2010). Development and face validity testing of a three-dimensional myringotomy simulator with haptic feedback. Journal of Otolaryngology—Head & Neck Surgery 39 (2): 122–129.
Spicer MA, van Velsen M, Caffrey JP and Apuzzo ML (2004). Virtual reality neurosurgery: A simulator blueprint. Neurosurgery 54 (4): 783–797, discussion 788–797.
Stredney D et al (2002). Temporal bone dissection simulation—An update. Studies in Health Technology and Informatics 85: 507–513.
Thomas G, Johnson L, Dow S and Stanford C (2001). The design and testing of a force feedback dental simulator. Computer Methods and Programs in Biomedicine 64 (1): 53–64.
Tolsdorff B et al (2007). Preoperative simulation of bone drilling in temporal bone surgery. International Journal of Computer Assisted Radiology and Surgery 2 (Suppl 1): 160–180.
Tolsdorff B et al (2010). Virtual reality: A new paranasal sinus surgery simulator. The Laryngoscope 120 (2): 420–426.
Urbankova A (2010). Impact of computerized dental simulation training on preclinical operative dentistry examination scores. Journal of Dental Education 74 (4): 402–409.
Vloeberghs M, Glover A, Benford S, Jones A, Wang P and Becker A (2007). Virtual neurosurgery, training for the future. British Journal of Neurosurgery 21 (3): 262–267.
Vozenilek J, Huff J and Reznek M (2004). See one, do one, teach one: Advanced technology in medical education. Academic Emergency Medicine 11 (11): 1149–1154.
Westebring-van der Putten E, Goossens R, Jakimowicz J and Dankelman J (2008). Haptics in minimally invasive surgery-a review. Minimally Invasive Therapy & Allied Technologies 17 (1): 3–16.
Wiet GJ, Schmalbrock P, Powell K and Stredney D (2005). Use of ultra-high-resolution data for temporal bone dissection simulation. Journal of Otolaryngology—Head & Neck Surgery 133 (6): 911–915.
Wiet GJ, Stredney D, Sessanna D, Bryan JA, Welling DB and Schmalbrock P (2002). Virtual temporal bone dissection: An interactive surgical simulator. Journal of Otolaryngology—Head & Neck Surgery 127 (1): 79–83.
Zhang L, Chen W, Ebert DS and Peng Q (2007). Conservative voxelization. The Visual Computer 23 (9): 783–792.
Ziv A, Wolpe P, Small S and Glick S (2003). Simulation-based medical education: An ethical imperative. Academic Medicine 78 (8): 783–788.
Acknowledgements
The authors wish to thank Alexandra Pearce for assistance with the preparation of the manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ruthenbeck, G., Reynolds, K. Virtual reality for medical training: the state-of-the-art. J Simulation 9, 16–26 (2015). https://doi.org/10.1057/jos.2014.14
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1057/jos.2014.14