Abstract
Outdoor air pollution, largely from fossil fuel burning, is a major cause of morbidity and mortality in the United States, costing billions of dollars every year in health care and loss of productivity. The developing fetus and young child are especially vulnerable to neurotoxicants, such as polycyclic aromatic hydrocarbons (PAH) released to ambient air by combustion of fossil fuel and other organic material. Low-income populations are disproportionately exposed to air pollution. On the basis of the results of a prospective cohort study in a low-income population in New York City (NYC) that found a significant inverse association between child IQ and prenatal exposure to airborne PAH, we estimated the increase in IQ and related lifetime earnings in a low-income urban population as a result of a hypothesized modest reduction of ambient PAH concentrations in NYC of 0.25 ng/m3. For reference, the current estimated annual mean PAH concentration is ~1 ng/m3. Restricting to NYC Medicaid births and using a 5 per cent discount rate, we estimated the gain in lifetime earnings due to IQ increase for a single year cohort to be US$215 million (best estimate). Using much more conservative assumptions, the estimate was $43 million. This analysis suggests that a modest reduction in ambient concentrations of PAH is associated with substantial economic benefits to children.
Similar content being viewed by others
Introduction
In addition to their impacts on health, the economic cost of environmentally-related disease in US children is estimated to be $76.6 billion,1, 2 and for neurobehavioral disorders related to environmental pollutants $9.2 billion.3 Here we have estimated the economic cost of prenatal exposure to a component of air pollution, polycyclic aromatic hydrocarbons (PAH), and the economic benefit of a modest reduction in ambient concentrations of the pollutants. The estimate is based on a damage function derived from a prospective cohort study in New York City (NYC), the Columbia Center for Children’s Environmental Health (CCCEH) cohort study.
PAH are widespread urban pollutants released to the air during incomplete combustion of fossil fuel, tobacco, and other organic material. Urban minority populations represent high-risk groups both for disproportionate exposure to air pollution and for adverse health and developmental outcomes.4, 5, 6, 7, 8 Environmental exposures during the prenatal and early postnatal stages are of particular concern because of the heightened susceptibility of fetuses and infants to diverse environmental pollutants, including neurotoxicants such as PAH.9, 10, 11, 12 PAH, such as benzo[a]pyrene (BaP), have been shown to be neurodevelopmental toxicants in experimental and epidemiological studies involving prenatal exposure.13, 14
In the CCCEH cohort study, prenatal exposure to airborne PAH was associated with developmental delay at 3 years of age,15 reduced child IQ at 5 years of age,16 and behavioral problems at 7 years of age.13 The present analysis is based on CCCEH results for the association between prenatal PAH exposure and IQ. Change in IQ has been used by Grosse and colleagues to estimate gains in lifetime earnings for each year’s US cohort as a result of reduced exposure to lead (from $110 billion to $319 billion per year) and by Trasande and colleagues to estimate the lost economic productivity of US children attributable to mercury emissions from American power plants ($1.3 billion, range = $0.1–6.5 billion) each year.17, 18 Here, by focusing on a prevalent environmental exposure in a low-income population of pregnant women and their children, this article provides new policy-relevant data.
Methods
Data from the CCCEH cohort study provided the damage function for PAH and IQ
As previously described, the cohort comprised children of nonsmoking African-American or Dominican-American women and their children residing in Washington Heights, Harlem, or the South Bronx in NYC, who were followed from in utero to 5 years of age.16 Prenatal personal air monitoring of eight nonvolatile PAH, including BaP was carried out during the third trimester of pregnancy over a 48-hour period as described.16 Total PAH exposure was defined as the summation of these eight PAH. Prenatal and postnatal questionnaires were administered to the mothers to obtain demographic, residential, history, health, and environmental data. At the age of 5 years, 249 children were assessed using the Wechsler Preschool and Primary Scale of Intelligence-Revised (WPPSI-R). We used multiple linear regression models to test the associations between prenatal PAH levels (using a dichotomous measure or continuous (Ln) transformed PAH) and IQ, accounting for factors other than PAH exposures that are known to affect intellectual development. The associations between the continuous measure of PAH exposure and IQ scores were significant (full-scale IQ: β −3.00; P=0.009; verbal IQ: β −3.53; P=0.002). The observed decrease in full-scale IQ in the CCCEH cohort among children above the median PAH exposure level compared with less exposed children was similar to that reported for children with lifetime average blood lead concentrations between 5 and 9.9 μg/dL compared with less exposed children.19
Calculation of the cost of PAH-related IQ reduction
To derive estimates of the cost of IQ reduction attributable to prenatal PAH exposure, we followed the method used by Grosse and colleagues and Trasande and colleagues in their assessments of lead and mercury, respectively.17, 18 We first calculated the estimated gain in IQ corresponding to the hypothesized reduction in ambient PAH exposure of 0.25 ng/m3. For context, the mean ambient PAH level measured in several studies of outdoor/ambient urban air in the United States was ~1 ng/m3. Data on ambient levels of PAH in Los Angeles (1998–2002)20 and recent data (unpublished, courtesy of Rachel Miller, MD) from a single stationary air monitor at West 168th and Broadway, NYC, showed average ambient levels to be about 1 ng/m3 in both cities. Subtracting the mean indoor level of PAH monitored over several weeks in the homes of women participating in the CCCEH cohort study (2.08 ng/m3)21 from the women’s personal monitored mean level (3.13 ng/m3) gives an estimated outdoor exposure concentration of ~1.00 ng/m3. However, the mean personal air concentration of nonvolatile PAH in our cohort study (3.13 ng/m3) reflected both indoor and outdoor exposures to PAH, not only because the daily activities of the women took place in both environments, but also because the indoor concentration of nonvolatile PAH resulted in large part from the transport of outdoor air into the indoor environment.22, 23
To estimate the size of the population at risk in NYC, we followed Weiland and colleagues24 and selected Medicaid births in NYC which shared basic socioeconomic characteristics of the CCCEH cohort. In the absence of data from personal monitoring of PAH in other segments of the population in the city, we were unable to select a population known to have the same personal exposure to PAH. However, the analysis is broadly relevant to policy on air pollution because PAH exposure is ubiquitous in the urban environment from fossil fuel burning, especially traffic. City-wide monitoring data showed variability in concentrations across the area, with pollution levels generally higher in lower income areas,25 supporting the selection of the Medicaid population as the population at risk.
The total number of births in NYC in 2002 was 122 937 of which 63 462 were births to women on Medicaid.26 We assumed comparable exposure to PAH during pregnancy as in the CCCEH cohort. For a single NYC birth cohort on Medicaid, we multiplied the estimated gain in IQ per hypothesized reduction in PAH exposure (above) by the estimated gain in earnings per IQ point (seeTable 1).
For our ‘best-case’ (Case 1) estimate of the benefit of reducing PAH levels, we assumed that one IQ point results in a 1.1 per cent increase in earnings based on Grosse27 who reviewed all studies on IQ points and annual earnings through 2007. For our Case 2 (lower bound) estimate, we applied the lower end value of a 0.85 per cent increase in earnings based on Heckman and colleagues.28 We used the published estimate of discounted lifetime earnings (in year 2000 US$) for a 2-year-old member of the birth cohort.17 This is reasonable since most of the CCCEH cohort was enrolled over a period of several years spanning 2000. Our primary analysis used a 5 per cent discount rate; we have also provided an analysis using a 3 per cent discount rate.
Results
On the basis of our prior study,16 a one LnPAH unit decrease is associated with a 3 point increase in IQ. Assuming log linearity of dose-response (based on our data), the effect on IQ of a specified reduction in PAH exposure can be calculated as:

where β=−3. The IQ regression model is IQ=α+β∗log(PAH)=α−3.0∗log(PAH).
With two levels of PAH and two levels of IQ:

So:

For a reduction of 0.25 ng/m3, the best estimate of the gain in IQ is 0.86 point (−3∗log[1/0.75]). The lower bound of the effect of PAH on IQ is  . Using the lower bound estimate of the PAH effect, the gain in IQ corresponding to a reduction of 0.25 ng/m3 is 0.22 point (−0.77∗log[1/0.75]).
. Using the lower bound estimate of the PAH effect, the gain in IQ corresponding to a reduction of 0.25 ng/m3 is 0.22 point (−0.77∗log[1/0.75]).
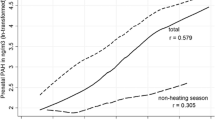
On the basis of Grosse and colleagues,17 we estimated the effect of one IQ point on lifetime earnings in our selected population. Grosse and colleagues used an estimate of the present value (PV) of future lifetime earnings (in year 2000 US$) for a 2-year-old child, calculated using a 3 per cent discount rate ($723 300), a 5 per cent discount rate ($353 400), and a 0 per cent discount rate. We have provided results using 5 per cent and 3 per cent discount rates as recommended by an expert panel convened by the US Public Health Service29. Our primary analysis (seeTable 1) was based on the 5 per cent discount rate; in the text we also summarize the results based on the 3 per cent discount rate.
The lifetime economic gain for each year’s birth cohort as a result of the specified decrease in PAH exposure is given inTable 1. For a reduction of 0.25 ng/m3 PAH in air, for each annual cohort of NYC Medicaid births, the Case 1 estimate is $215 million; and the Case 2 estimate is $43 million. The Case 1 estimate corresponds to a 0.96 per cent increase in total earnings per person (3382/353 400); the Case 2 estimate corresponds to a 0.18 per cent increase in total earnings per person (671/353 400).
With a 3 per cent discount rate, the PV of lifetime earnings was calculated to be $723 300.17 Using a 3 per cent discount rate, the Case 1 estimate of the benefit per cohort of a reduction of 0.25 ng/m3 PAH (in 2000US$) is $441 million; the Case 2 estimate is $87 million.
Discussion
This analysis estimates substantial gains in earnings associated with a modest reduction in ambient PAH concentrations, hence in prenatal exposure, for each annual cohort of Medicaid births in NYC. Given the paucity of data available on the cost of environmentally related neurodevelopmental effects, we view our findings as a useful departure point for future researchers as well as policymakers, who often need to act in the face of uncertainty.
Our study has several limitations. We have defined our population at risk as one with similar demographic characteristics as our study cohort; that is, the NYC Medicaid population. However, the CCCEH cohort excludes smokers and those with other serious medical conditions, so if these factors interact with PAH on risk of IQ loss, our findings may underestimate the effect of exposure on IQ. As PAH are ubiquitous in urban environments, IQ and related earnings benefits are likely to accrue to other groups as well, although their impacts may be smaller than estimated here for a low-income population. Further, the present analysis does not consider other potential benefits of exposure reduction such as reduction of asthma and cancer risk which have been associated with PAH and diesel exposure.30, 31 Another limitation is that, although the present estimates of the association between prenatal PAH exposure and IQ are based on a peer-reviewed study that controlled for a number of important confounding factors, we cannot rule out the possibility of unmeasured confounding. Further, the models used to assess PAH impacts did not account for exposures to mercury and lead which may contribute to overestimation.
WPPSI-R verbal and full-scale IQ scores during the preschool period have been shown in many studies to be predictive of subsequent elementary school performance32, 33 and lifetime earnings.27 However, while IQ provides the best documented relationship with economic criteria, there are a number of limitations to IQ as an outcome, including the difficulty in estimating the full impact of cognitive ability on earning potential.17 Neurotoxins can influence both cognitive and non-cognitive ability; so economic analyses of the effects of reducing neurotoxin exposures on cognitive ability alone can understate the overall economic benefit.
There are a number of approaches for reducing PAH emissions including fuel efficiency and conservation, innovations in emissions control technology, and use of alternative fuels. However, an assessment of the costs of controlling emissions of PAH from diverse sources is beyond the scope of this analysis.
To the best of our knowledge, this is the first study to estimate the costs of IQ loss associated with PAH exposure and the corresponding benefits of PAH exposure reduction. It adds to the prior literature on economic costs of particulate air pollution that estimated sizable costs of the attributable morbidity and mortality.2, 34, 35, 36, 37
Our analysis suggests that a small reduction in ambient PAH would be associated with substantial economic benefits as measured by increased lifetime earnings. Next steps in research include a more comprehensive accounting of the impacts of air pollution, going beyond the narrow outcome of reduction of IQ to include broader neurotoxic, respiratory, and carcinogenic effects and also considering the effects of early exposure over the lifecourse.
References
American Lung Association. (2013) State of the Air 2013 Report.
Trasande, L. and Liu, Y. (2011) Reducing the staggering costs of environmental disease in children, estimated at $76.6 billion in 2008. Health Affairs (Millwood) 30 (5): 863–870.
Landrigan, P.J., Schechter, C.B., Lipton, J.M., Fahs, M.C. and Schwartz, J. (2002) Environmental pollutants and disease in American children: Estimates of morbidity, mortality, and costs for lead poisoning, asthma, cancer, and developmental disabilities. Environmental Health Perspectives 110 (7): 721–728.
Olden, K., Ramos, R.M. and Freudenberg, N. (2009) To reduce urban disparities in health, strengthen and enforce equitably environmental and consumer laws. Journal of Urban Health 86 (6): 819–824.
Perera, F.P. et al (2002) The challenge of preventing environmentally related disease in young children: Community-based research in New York City. Environmental Health Perspectives 110 (2): 197–204.
Claudio, L., Tulton, L., Doucette, J. and Landrigan, P.J. (1999) Socioeconomic factors and asthma hospitalization rates in New York City. Journal of Asthma 36 (4): 343–350.
Federico, M.J. and Liu, A.H. (2003) Overcoming childhood asthma disparities of the inner-city poor. Pediatric Clinics of North America 50 (3): 655–675.
New York City Department of Health. (1998) Vital Statistics. New York City: New York City Department of Health.
NRC. (1993) Pesticides in the Diets of Infants and Children. Washington DC: National Academy Press.
Perera, F.P. et al (2004) Biomarkers in maternal and newborn blood indicate heightened fetal susceptibility to procarcinogenic DNA damage. Environmental Health Perspectives 112 (10): 1133–1136.
World Health Organization. (1986) Principles for Evaluating Health Risks from Chemicals During Infancy and Early Childhood: The Need for a Special Approach. Environmental Health Criteria 59. Geneva, Switzerland: World Health Organization.
Grandjean, P. and Landrigan, P.J. (2006) Developmental neurotoxicity of industrial chemicals. Lancet 368 (9553): 2167–2178.
Perera, F.P. et al (2012) Prenatal polycyclic aromatic hydrocarbon (PAH) exposure and child behavior at age 6–7. Environmental Health Perspectives 120 (6): 921–926.
Wormley, D.D. et al (2004) Inhaled benzo(a)pyrene impairs long-term potentiation in the F1 generation rat dentate gyrus. Cellular and Molecular Biology (Noisy-le-grand) 50 (6): 715–721.
Perera, F.P. et al (2006) Effect of prenatal exposure to airborne polycyclic aromatic hydrocarbons on neurodevelopment in the first 3 years of life among inner-city children. Environmental Health Perspectives 114 (8): 1287–1292.
Perera, F.P. et al (2009) Prenatal airborne polycyclic aromatic hydrocarbon exposure and child IQ at age 5 years. Pediatrics 124 (2): e195–e202.
Grosse, S.D., Matte, T.D., Schwartz, J. and Jackson, R.J. (2002) Economic gains resulting from the reduction in children’s exposure to lead in the United States. Environmental Health Perspectives 110 (6): 563–569.
Trasande, L., Landrigan, P.J. and Schechter, C. (2005) Public health and economic consequences of methyl mercury toxicity to the developing brain. Environmental Health Perspectives 113 (5): 590–596.
Jusko, T.A., Henderson, C.R., Lanphear, B.P., Cory-Slechta, D.A., Parsons, P.J. and Canfield, R.L. (2008) Blood lead concentrations<10 microg/dL and child intelligence at 6 years of age. Environmental Health Perspectives 116 (2): 243–248.
Pleil, J.D., Vette, A.F., Johnson, B.A. and Rappaport, S.M. (2004) Air levels of carcinogenic polycyclic aromatic hydrocarbons after the World Trade Center disaster. Proceedings of the National Academy of Sciences of the United States of America 101 (32): 11685–11688.
Rundle, A.H. et al (2012) Association of childhood obesity with maternal exposure to ambient air polycyclic aromatic hydrocarbons during pregnancy. American Journal of Epidemiology 175 (11): 1163–1172.
Choi, H. et al (2008) Estimating individual-level exposure to airborne polycyclic aromatic hydrocarbons throughout the gestational period based on personal, indoor, and outdoor monitoring. Environmental Health Perspectives 116 (11): 1509–1518.
Naumova, Y.Y. et al (2002) Polycyclic aromatic hydrocarbons in the indoor and outdoor air of three cities in the U.S. Environmental Science and Technology 36 (12): 2552–2559.
Weiland, K., Neidell, M., Rauh, V. and Perera, F. (2011) Cost of developmental delay from prenatal exposure to airborne polycyclic aromatic hydrocarbons. Journal of Health Care for the Poor and Underserved 22 (1): 320–329.
The New York City Department of Health and Mental Hygiene. (2009) The New York city community air survey: Results from year one monitoring 2008–2009 Stevens L.M. (ed.) New York: New York City Health Department.
Li, W., Kelley, D. and Kennedy, J. (2003) Summary of Vital Statistics 2002: NYC Department of Health and Mental Hygiene.
Grosse, S.D. (2007) How much does IQ raise earnings? Implications for regulatory impact analyses. Association of Environmental and Resource Economists (AERE) 27 (2): 44.
Heckman James, J., Stixrud, J. and Urzua, S. (2006) The effects of cognitive and noncognitive abilities on labor market outcomes and social behavior. Journal of Labor Economics 24 (3): 411–482.
Gold, M.R., Siegel, J.E., Russel, L.B. and Weinstein, M.C. (eds.) (1996) Cost Effectiveness in Health and Medicine. New York: Oxford University Press.
Miller, R.L. et al (2004) Polycyclic aromatic hydrocarbons, environmental tobacco smoke, and respiratory symptoms in an inner-city birth cohort. Chest 126 (4): 1071–1078.
Bostrom, C.E. et al (2002) Cancer risk assessment, indicators, and guidelines for polycyclic aromatic hydrocarbons in the ambient air. Environmental Health Perspectives 110 (Supplement 3): 451–488.
Kaplan, C. (1996) Predictive validity of the WPPSI-R: A four year follow-up study. Psychology in the Schools 33 (3): 211–220.
Lemelin, J. P. et al (2007) The genetic-environmental etiology of cognitive school readiness and later academic achievement in early childhood. Child Development 78 (6): 1855–1869.
Sheffield, P., Roy, A., Wong, K. and Trasande, L. (2011) Fine particulate matter pollution linked to respiratory illness in infants and increased hospital costs. Health Affairs (Millwood) 30 (5): 871–878.
Kan, H. and Chen, B. (2004) Particulate air pollution in urban areas of Shanghai, China: Health-based economic assessment. Science of the Total Environment 322 (1–3): 71–79.
Zhang, M., Song, Y. and Cai, X. (2007) A health-based assessment of particulate air pollution in urban areas of Beijing in 2000–2004. Science of the Total Environment 376 (1–3): 100–108.
Pérez, L., Sunyer, J. and Künzli, N. (2009) Estimating the health and economic benefits associated with reducing air pollution in the Barcelona metropolitan area (Spain). Gaceta Sanitaria 23 (4): 287–294.
Acknowledgements
The National Institute of Environmental Health Sciences (grants 5P01ES09600, 5R01ES08977), the US Environmental Protection Agency (R827027, RD832141, RD83450901), the John and Wendy Neu Family Foundation, the John Merck Fund, the Blanchette Hooker Rockefeller Foundation, and the New York Community Trust supported this study. The authors also thank Dr Julien Teitler, Irwin Garfinkel, Barbara Simons, and Sara Tjossen for their helpful comments.
Author information
Authors and Affiliations
Corresponding author
Additional information
A careful look at exposures to airborne polycyclic aromatic hydrocarbons, helped the authors estimate the effect on the IQ of children in New York City. They estimate the benefits of reducing exposures.
Rights and permissions
About this article
Cite this article
Perera, F., Weiland, K., Neidell, M. et al. Prenatal exposure to airborne polycyclic aromatic hydrocarbons and IQ: Estimated benefit of pollution reduction. J Public Health Pol 35, 327–336 (2014). https://doi.org/10.1057/jphp.2014.14
Published:
Issue Date:
DOI: https://doi.org/10.1057/jphp.2014.14